Whiplash injuries can turn even the simplest head movement into a sharp reminder of trauma. Sudden acceleration–deceleration forces, often from rear‑end collisions, jolt the cervical spine into an S‑shaped curve before a rebound snap straightens it again. The result is overstretched muscles, strained ligaments, and sometimes subtle shifts in vertebral position. While ice packs and pain relievers soothe the immediate ache, proper recovery hinges on one deceptively simple goal: regaining healthy spinal alignment. By purposefully re‑centering the cervical curve, you restore balanced load distribution, ease muscle guarding, and create the biological conditions nerves and soft tissues need to heal. In other words, alignment is the quiet engine driving lasting whiplash recovery.
What Happens to Your Spine During Whiplash?
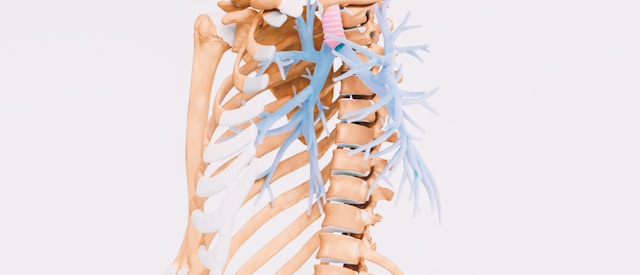
During the first 150 milliseconds of impact, the lower cervical vertebrae extend while the upper vertebrae flex, producing an “S‑curve” that momentarily reverses the neck’s natural lordosis. Ligaments stretched beyond their elastic limit may fail to rebound fully, leaving minor, meaningful positional faults between vertebrae. Researchers have measured post‑crash losses of 12–15 degrees of lordotic curvature, accompanied by forward head translation and muscle spasm that splints the region in painful rigidity.
These micro‑misalignments set off a chain reaction. Altered joint mechanics trigger abnormal afferent signaling, keeping cervical muscles in a protective but exhausting state of contraction. Blood flow decreases, metabolic waste accumulates, and pain sensitization ramps up. Left uncorrected, the faulty posture progresses to chronic myofascial pain or cervicogenic headache months later. Modern clinical guidelines emphasize early, gentle mobilization and alignment‑focused therapy over the outdated “neck brace and rest” approach.
Why Proper Alignment Accelerates Healing
Pain reduction is only the surface benefit of restoring the cervical curve. When vertebrae resume their standard arc, facet joints glide instead of jamming, and discs regain symmetrical loading. This mechanical harmony reopens nutrient pathways that cartilage depends on for diffusion‑based nourishment. Simultaneously, balanced posture lessens tensile stress on already inflamed anterior longitudinal and alar ligaments.
Clinical trials illustrate the payoff. A 2024 randomized study compared 59 patients receiving specific cervical adjustment techniques to 60 patients following a conventional strengthening program. The adjustment group logged significantly larger gains in range of motion and twice the drop in pain scores, even though they attended only three sessions versus twenty in the control cohort. Radiographs confirmed measurable restoration of lordosis, underscoring that structural change, not session quantity, predicted symptom relief.
Another prospective case series using Chiropractic BioPhysics (CBP) protocols documented an average 15‑degree curvature recovery and 23 percent reduction in disability after nine weeks. Importantly, these gains persisted at six‑month follow‑up, suggesting that once alignment is re‑established, soft‑tissue remodeling maintains it.
Evidence‑Based Alignment Techniques and Exercises
Upper‑cervical specific adjustments. Practitioners trained in atlas‑axis correction use low‑force vectored impulses to realign C1 and C2. Minor angle corrections can produce significant global changes because these segments house the brainstem and dictate downstream posture. Recent observational data show meaningful pain relief within two to four visits, with no serious adverse events reported.
Cervical extension traction. CBP and similar methods employ seated or supine traction devices that gently restore lordotic curvature over 10–20 sessions. By placing the neck into a controlled extension bias for timed intervals, viscoelastic creep allows shortened anterior tissues to lengthen while posterior tissues relax.
Guided neck‑specific exercise therapy. Not all alignment work requires external devices. A 2024 meta‑analysis found that therapist‑guided deep cervical flexor training (think chin tucks and graded head lifts) outperformed unstructured home programs in reducing both pain intensity and disability. Key is the “guided” component—real‑time feedback helps patients activate stabilizers without recruiting superficial, pain‑provoking muscles.
Progressive mobility drills. Once acute pain subsides, controlled rotations, lateral flexions, and scapular retractions expand motion arcs and reinforce the new alignment. Therapists often integrate resisted band rows and thoracic extension work to correct the rounded‑shoulder posture perpetuating forward head carriage.
Building a Long‑Term Alignment Routine at Home
Recovery does not end when formal therapy concludes. Daily habits either protect or erode the cervical curve you just reclaimed. Begin each morning with five slow chin tucks, pausing two seconds at full retraction; add gentle side glides to train symmetry. Pair computer or smartphone sessions with “20‑20 posture breaks”: every twenty minutes, spend twenty seconds standing tall, shoulder blades drawn down, eyes level.
Ergonomic tweaks help too. Position monitors so the top third sits at eye height, and keep screens an arm’s length away to curb craning. When driving, adjust the headrest so it meets the base of the skull, and tilt mirrors just enough that slouching makes them unusable—instant feedback.
Sleep is when connective tissues remodel, so choose a pillow supporting cervical lordosis. Memory‑foam designs with a gentle contour work well for most back sleepers, while side sleepers do better with a thicker edge that fills the shoulder‑to‑ear gap. Rotate pillows every year; compressed foam loses shape and invites micro‑misalignment.
Finally, maintain general fitness. Aerobic exercise improves cervical blood flow, and strength work targeting scapular stabilizers prevents the rounded‑shoulder pattern linked to chronic neck strain. Think rows, reverse flys, and farmer’s carries—movements that teach shoulders to sit back and down.
Spinal alignment is not an optional add‑on but the foundation of effective whiplash recovery. Micro‑misalignments amplify pain, delay tissue repair, and foster chronic dysfunction. Yet targeted adjustments, traction‑based curve restoration, and guided stabilization exercises can correct these faults, often within weeks. Consolidating gains through posture‑smart habits keeps your neck in its natural arc, letting ligaments and discs remodel instead of relapse. Partner with a clinician who measures curvature objectively, sets alignment as a primary goal, and teaches you how to defend it daily. Your future self—able to check blind spots, hug loved ones, and sleep without a second thought—will thank you for the precision now.